-
-
Like what you see?
LetsTalkUrl
Let's Talk
COVID-19 has compelled the modern, connected society to live in physical isolation. It has impacted public health, disrupted operations, and made it extremely difficult to manage resources. Health systems of several countries have had to ration critical medical supplies like respirators, masks and gloves.
Best-practices from past outbreaks like the SARS in 2003, MERS and Ebola have proven to be inadequate, but effective use of digital technologies can help fight this pandemic, and any future public health crises more effectively.
This article discusses four such digital technologies that can transform operations for public health agencies, enabling them to respond early to contain any future epidemic and deliver the right services to the population that demands the most care during crisis.
The magnitude of COVID-19 outbreak requires agencies to radically rethink how to adopt digital technologies to make interventions more responsive and improve outcomes for the population they serve.
Agencies need to start implementing high speed, high touch digital technologies across their process chain to bring more structure and visibility to their population health initiatives, and quickly adapt to the scale and scope of changes required by pandemics like the COVID-19.
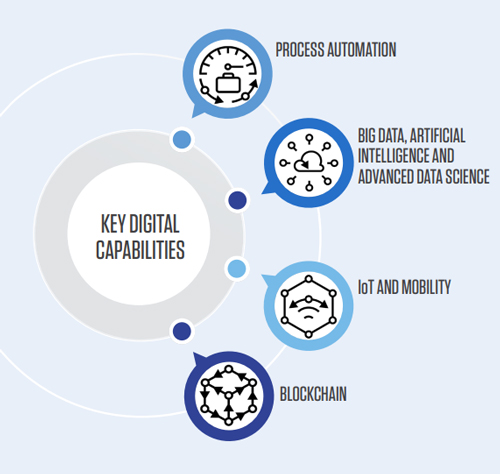
COVID-19 will begin a renaissance for public health IT. Government healthcare agencies, through strategic interventions and cross agency collaboration, should operationalize the following key digital capabilities. This will allow them to deliver various health and social programs in a coordinated and uninterrupted manner to the population that needs them the most.
There is a significant shortage of health and human services staff/manpower due to lockdowns and physical distancing measures. Agencies are focused on providing lifesaving and life-enhancing services. However, certain operational or administrative tasks like new provider enrollment, processing health care data, administering benefit applications, eligibility determination, identity verifications, etc. also become mission critical, especially to deliver timely services to the most vulnerable population.
For all these administrative tasks, process automation robots can be programmed to take care of repetitive functions, minimize the impact of labor shortages and ensure that operations run uninterrupted.
Fighting pandemics like COVID-19 requires real time sharing of lab testing, supplies, and hotspots information with various agencies, departments and stakeholders. Handling and triaging this information manually is effort intensive, prone to errors and can lead to backlogs.
Through process automation bots, agencies can programmatically capture this information (e.g., lab test results), compile and share/link them with hospital EMRs, vital record management systems, Clinical Research Organizations, the CDC, and state and local health departments for effective tracking and planning of medical care for COVID-19 impacted patients.
This end-to-end process automation will accelerate response management, even when agencies are short-staffed.
CMS granted section 1135 waivers to certain states for provider enrollment to support the 2019-Novel Corona virus national emergency. This means waiving screening requirements including criminal background checks, credentials,verification, and address validation through site visits, etc. This approach is not without risk. Alternatively, this is an opportunity for public health agencies to leverage process automation techniques enabled with Optical Character Recognition and Natural Language Processing to capture and compile information on provider demographics, identifiers (NPI/SSN/ EIN/TIN), and group and product data. This information will help state agency staff complete background research more accurately, in less time, through fewer manual interventions, leading to a streamlined and expedited provider enrollment process in an emergency situation like COVID-19.
Also Read:
These are just a few examples. Automation capabilities can be extended to various other business functions as well like identity and eligibility verification, prior authorizations, medical necessity checks, unemployment application processing, supply chain management, etc. With this support, agencies can run business as usual with greater speed, accuracy, and efficiency especially in public health emergencies like the one we are facing today.
Despite epidemics like the flu and the HIV, pandemics like the Avian Influenza H7N9, and natural disasters like Katrina, public health data infrastructure remains underfunded and underdeveloped.
It has always been a challenge to obtain the right intelligence at the right time to initiate timely measures like bio- surveillance, vaccine campaigns, travel restrictions, allocation of medical supplies, optimization of resource capacity, triaging care, implementing targeted public health interventions and cross-agency collaboration.
The recent COVID-19 stimulus package grants over $500M to public health data surveillance and infrastructure modernization that can help address this issue and enable states to develop the right data and analytics tools to fight pandemics like the COVID-19.
Agencies must eliminate their sluggish and burdensome data systems and replace them with integrated, scalable, advanced analytics driven, multi-modal data systems that are connected with laboratories, healthcare facilities and public health authorities (federal, state and local) for fast and reliable sharing of data and intelligence to protect every citizen from health threats.
Pathogens like COVID-19 generate a lot of patient-related data; e.g., symptoms that get captured by mobile/IoT devices (thermometer guns, smart phone apps), diagnostic reports (chest CT scans, lab results), remote care monitoring systems, social media posts, patient movement patterns, etc. All this information can be aggregated and managed in an interoperable cloud based Big Data and hybrid data storage systems. It can be analyzed using advanced data science techniques (AI, Machine learning, Deep Learning) to provide real time intelligence (descriptive, diagnostic, predictive and prescriptive) to public health stakeholders, improving their ability to proactively arrest the spread of the disease and prepare better for any future waves. The intelligence obtained from this data eco- system will provide public health agencies with near real time ability to monitor and manage various initiatives including:

The use of social determinants of health attributes can further help refine and plan for high risk population identification based on their socio-behavioral, attitudinal risk composites, e.g., level of community engagement, availability of relatives and neighborhood resources as care givers, access to care facilities, transportation access, education, financial health, home status, food insecurity, etc.
To overcome this long standing public health disadvantage, the need of the hour is to adopt sophisticated data analytics techniques and tools that can transform, sustain and strengthen agencies with data and intelligence that drive organizational capacity for public health improvement and efficiency and establish a foundation in preparation for any future coronavirus waves or epidemic episodes.

Mobility and IoT have long been a way of life for caregivers and the patients in nearly all aspects of a healthcare ecosystem. But, the real value of these devices in public health is only now being realized.
Today, a lot of patient generated data on COVID-19 is being transmitted through mobile devices (health screening apps, digital health coach apps, virtual assistants like Alexa, Siri apps, social media apps, GPS, etc.) and IoT devices (e.g. telemetry, digital thermometers, digital spirometer, glucometers, digital BP monitors, drone captured surveillance data etc.).
In an epidemic/pandemic situation, these devices can rapidly provide a range of useful functional capabilities such as real time data capture, time series analysis of data and generation of actionable insights,e.g. COVID-19 case detection and contact tracing. The value is amplified because of low/zero touch design of these devices. Data can be uploaded to EMRs so that infected patients need not visit the hospital or medical center while still being attended to by personal physicians. Case status can be tracked and monitored through real time alerts to make sure that critical events like arrhythmias, asthmatic episodes, dyspnea, or diabetic attacks that can over complicate a COVID-19 infected patient can be responded to immediately.
A further innovative application of virtual/mobile healthcare technology can be the use of mini tele-ICU system to address critical care needs of patients in this pandemic and others in the future. Mini tele-ICU systems that use mobile and portable devices, simple Bluetooth telemetric monitors, and low cost ventilators can quickly and significantly expand capacity of health care providers. This lower-cost approach (compared to a real ICU bed care) will allow diagnostic, treatment, post-treatment, and quarantine services to be delivered across organizational, provincial, and national boundaries, perfectly aligning with the ‘doctors without borders’ paradigm.
These technologies minimize in-person patient monitoring workload, enabling the medical staff to handle more cases, facilitating continued communication and collaboration across organizational boundaries, providing the necessary mechanism for data driven intelligence to empower accurate diagnosis and prognosis decisions, and last but not the least, minimizing the chances of infection spread by keeping the frontline healthcare workers and patients safe from COVID-19 cross infection.
The universal use of the mobile, IoT enabled telehealth/remote patient monitoring/virtual care technologies in public health should have happened already. But, better late than never. Hence the recent bold action taken by the Federal Government (both through the CARES Act’s funding for telehealth adoption and CMS 1135 waiver authority for expanding Medicare’s telehealth benefits) will give people greater access to timely care for fighting the COVID-19 outbreak.
COVID-19 is compelling organizations to think out of the box. Technology like the Blockchain is an example of a tool that can address public health epidemics.
Blockchain technology can be used to augment supply chain and inventory management by tracking, verifying, and tracing medical supplies, drugs, food safety, or even fund movements and donations to support the COVID-19 pandemic. The benefits will also be realized beyond the crisis when agencies use this technology to replicate, share, and synchronize digital data spread across multiple sites to ensure true collaboration.
Public health agencies can use the technology to connect healthcare facilities with federal, state and local health agencies to transmit de-identified patient data showing COVID-19 virus- like symptoms in cities and counties where the virus has already spread or appears to be spreading. This data can be tracked and analyzed in real time to help agencies immediately spot the spread and implement proactive preventive measures in the identified areas by increasing the workforce, providing medical supplies- drug, test kits, masks, respirators, etc. and effective capacity planning.
In addition, when the concern is with the spread of the pathogen through people migration (especially when passengers are known to have traveled from countries that have already declared a state of emergency), the system can be used in real time to transmit passenger health screening data from the Port of Entry declaration systems to health authorities for more effective tracking and tracing. Based on the information, the passengers with positive COVID-19 symptom can then be designated as high-risk groups and obligated to visit medical institutions in order to be tested and quarantined if required.
Most of the pandemics/epidemics originate from livestock mistreatment. Hence, beyond COVID-19, public health agencies can use Blockchain technology to identify livestock origin, their management, associated biological risk level from region to region based on their origin, and mitigate chances of an outbreak.
The World Health Organization (WHO) recently partnered with Blockchain technology companies to launch a distributed ledger technology (DLT)- based platform for sharing data about the coronavirus pandemic. US public health agencies can adopt best-practices and learnings from this initiative as they plan their own Blockchain programs.

Aristotle famously said “It is during our darkest moments that we must focus to see the light.” COVID-19 is a dark cloud that has engulfed the world and the public health systems. This is also the time when we must remain strong and find the silver lining that can help us navigate through this disruption.
Time is of the essence in case of an outbreak. Sharp acumen and quick reactions become crucial for public health agencies to fight the problem. They need to keep the workforce active, motivated, and productive even as they are unable to reach their place of work, and enable them to serve the vulnerable population with the best healthcare and human services - the biggest need of the hour.
If agencies haven’t already implemented or made plans to adopt digital capabilities (emerging, new and existing) in the last few years, they should do that now. They should adopt mobile capabilities, enhance the use of automation, modernize existing data infrastructure for integrated, advanced analytics and AI functions, using Blockchain for real time tracking and visibility.
All of these technologies can be made cloud native which will be an incredibly powerful way to make healthcare operations more resilient, scalable, safe and simplified. And that’s not all, this technology will ensure high returns long after COVID-19 conditions improve and will enable agencies to be even more successful in delivering on their mission.
Digital transformation is not just about adopting new technology tools, solutions, and intellectual property. It’s about having the expertise in place to imagine and bring to life the full potential of the future.
